Have you, perhaps, heard the term "MS quad" and wondered what it truly means? It's almost as if this phrase points directly to a crucial aspect of Multiple Sclerosis, a condition that touches the lives of so many. This article is here to help you get a better grip on what Multiple Sclerosis, or MS, really is, and how it can, in a way, affect your body's ability to move, especially your limbs. We'll talk about the protective covering of nerves and what happens when it breaks down, which is, you know, a big part of the MS story.
Multiple sclerosis, as a matter of fact, is a condition where the body's own defense system, the immune system, starts to attack the protective covering around nerves. This covering, which is called myelin, is vital for sending messages quickly and smoothly throughout your brain and spinal cord. When this covering gets damaged, it's like frayed wires, making it harder for those messages to get where they need to go, and that, too, can lead to a whole host of physical challenges.
This damage can, in some respects, show up in many different ways for different people. You might experience a feeling of numbness, or a general weakness in your arms or legs, and sometimes, you know, even trouble walking steadily. There can also be changes in vision, which is, quite frankly, another common sign. Understanding these signs is a pretty important first step in recognizing the condition and seeking help.
Table of Contents
- What Exactly is MS?
- Recognizing the Signs: MS Symptoms
- Getting a Clear Picture: Diagnosing MS
- Different Paths: Types of MS
- Hope on the Horizon: MS Treatment and Management
- Living with MS: Everyday Realities
- Frequently Asked Questions About MS
What Exactly is MS?
Multiple sclerosis, which is also simply called MS, is a condition where your immune system, the body's natural defense, begins to attack the protective layer that surrounds the nerves in your brain and spinal cord. This vital covering, as I was saying, is known as myelin. Think of it like the insulation around an electrical wire; it helps signals travel quickly and efficiently. When this insulation gets damaged, signals can slow down, get distorted, or even stop completely, which, you know, causes problems throughout the body.
This attack on myelin leads to inflammation and damage, creating scars or lesions on the nerves. These lesions can be found in various spots throughout the central nervous system, and their location, apparently, determines which parts of the body are affected and what symptoms a person might experience. It's really quite a complex process, and the specific areas of damage can make each person's experience with MS pretty unique, which is, in fact, why it can be so tricky to pin down.
The brain and spinal cord are, naturally, the command centers for nearly everything your body does, from thinking and feeling to moving and seeing. So, when MS causes issues in these areas, the effects can be widespread and, you know, sometimes quite noticeable. It’s a condition that, in a way, disrupts the body's communication network, and understanding this basic mechanism is, quite frankly, key to understanding the challenges people face.
Recognizing the Signs: MS Symptoms
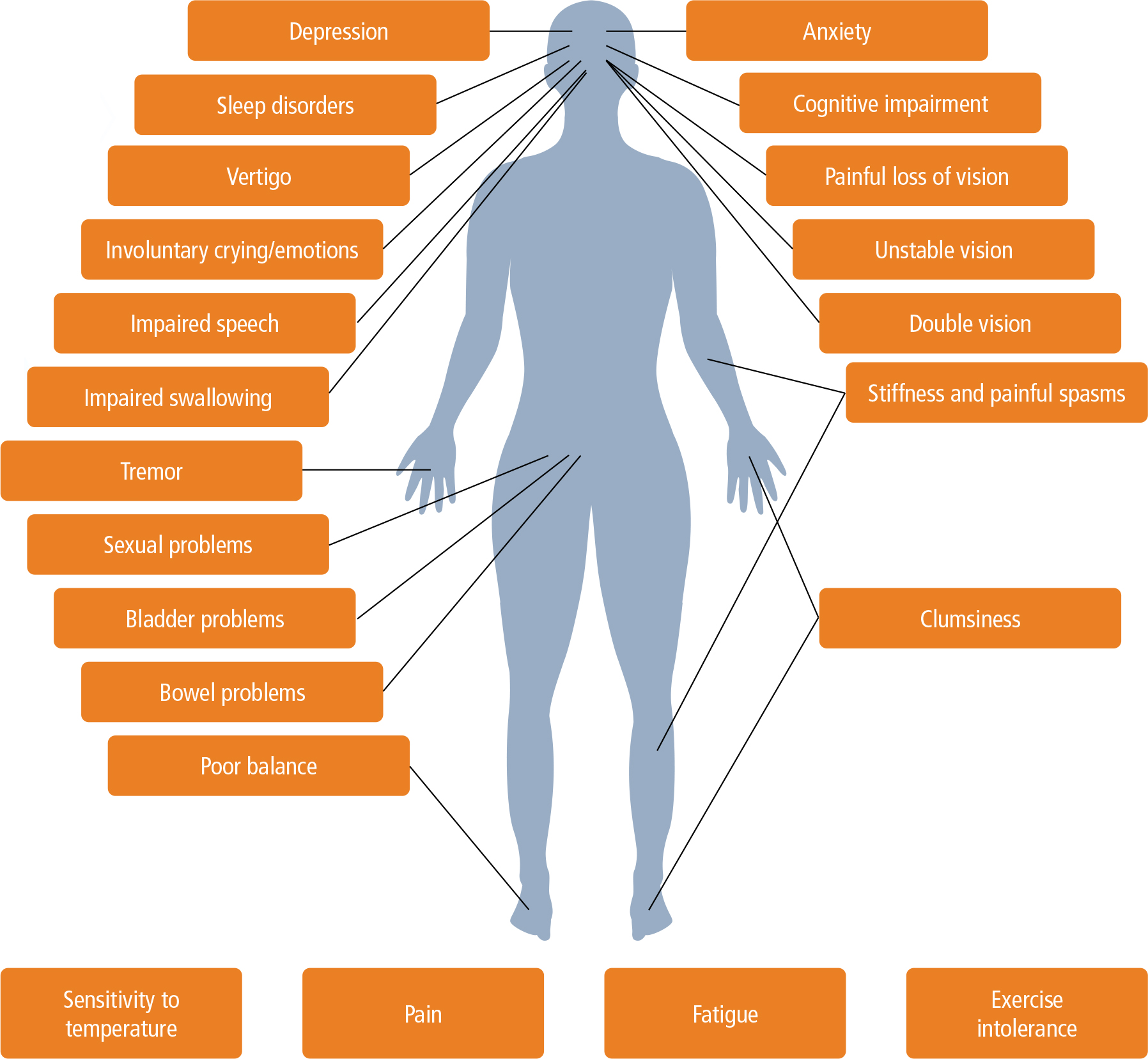
The symptoms of Multiple Sclerosis can be, as a matter of fact, quite varied, depending on which nerves are affected and how much damage has occurred. It's not uncommon for people to experience a range of physical feelings that can, you know, come and go or even get steadily worse over time. Some of the most common signs include a feeling of numbness, a noticeable weakness in your limbs, and, very often, some trouble with walking. Vision changes, too, can be a pretty early indicator for some individuals.
Imagine, for instance, trying to pick up a small object, and your fingers just don't quite feel right, or they seem to lack their usual strength. That's a bit like the numbness or weakness some people experience. Or consider walking across a room; for someone with MS, it might feel like their legs aren't quite cooperating, leading to a clumsy gait or, you know, a need for support. These kinds of sensations, which are, you know, sometimes subtle at first, can gradually become more pronounced.
Vision changes are also, quite literally, a common symptom. This could involve blurry vision, double vision, or even, in some cases, temporary loss of sight in one eye. These visual disturbances happen when the optic nerve, which carries information from the eye to the brain, is affected by the myelin damage. It's an important symptom to pay attention to, as it can, quite simply, be one of the first clues that something is amiss, and that, too, is why doctors often ask about it.
The "Quad" Connection: Mobility Challenges
When we talk about "MS quad," we're not using a formal medical term, but it really highlights how MS can impact the four limbs – your arms and, especially, your legs. A very common complaint among people living with MS is, in fact, weakness in their legs, which can make simple tasks like standing up or climbing stairs feel like a huge effort. This weakness often affects the quadriceps muscles, the large muscles at the front of your thighs, which are, naturally, crucial for walking and maintaining balance.
Trouble walking, or what doctors might call gait disturbance, is, quite literally, one of the most visible signs of MS for many. It can range from a slight unsteadiness to needing walking aids like canes or walkers. The nerve damage makes it harder for the brain to send clear, consistent messages to the muscles in the legs, which, you know, can lead to a feeling of heaviness or a lack of coordination. It's a very real challenge that affects daily life, and it's something that, you know, people often seek help for.
This impact on mobility can, in some respects, also lead to fatigue, which is another incredibly common and often debilitating symptom of MS. When your muscles have to work harder to do simple movements because of nerve damage, your body uses more energy, and that, quite simply, can leave you feeling utterly drained. So, the "quad" connection isn't just about muscle weakness; it's also about the broader energy cost of movement when living with MS, and that, too, is something people often don't consider.
Getting a Clear Picture: Diagnosing MS
Getting a diagnosis of MS isn't, in fact, always a straightforward process, mainly because there isn't one single, specific test that can definitively say, "Yes, this is MS." Instead, doctors typically piece together information from several different sources to make a clear determination. It's a bit like solving a puzzle, where each piece of information brings the full picture into better focus, and that, you know, takes time and careful consideration.
The diagnosis usually starts with a detailed look at your medical history. Your doctor will ask you, quite simply, about all the symptoms you've been experiencing, when they started, how long they lasted, and if they've come and gone. They'll also want to know about any previous health issues or, you know, family history that might be relevant. This conversation is, quite frankly, a very important first step in understanding your unique situation, and it really sets the stage for everything else.
Following the discussion, a physical exam is, naturally, a crucial part of the process. During this exam, the doctor will check your reflexes, balance, coordination, vision, and strength. They're looking for any subtle signs of nerve damage that might not be immediately obvious to you. For instance, they might ask you to walk in a straight line or touch your finger to your nose, which are, you know, simple ways to assess neurological function. This hands-on assessment provides very valuable clues.
Magnetic Resonance Imaging, or MRI, scans are, in fact, a cornerstone of MS diagnosis. These powerful imaging tests can reveal lesions or areas of damage in the brain and spinal cord, which are characteristic of MS. Doctors often look for new lesions or changes in existing ones over time, which can help confirm the diagnosis. It's a non-invasive way to see what's happening inside your central nervous system, and it's, quite simply, an incredibly helpful tool for doctors.
In some cases, a spinal tap, also known as a lumbar puncture, might be recommended. This procedure involves taking a small sample of cerebrospinal fluid (CSF), the fluid that surrounds your brain and spinal cord. The CSF is then analyzed for specific proteins or antibodies that can be present in people with MS. While not always necessary, a spinal tap can, in a way, provide additional evidence to support an MS diagnosis, especially when other tests are not entirely conclusive, and that, too, is why it's sometimes used.
So, a diagnosis of multiple sclerosis is given by a combination of medical history, a thorough physical exam, the results from MRIs, and, you know, sometimes, spinal tap results. It’s a comprehensive approach that helps ensure the most accurate possible diagnosis, which is, quite frankly, essential for getting the right care and support. It's a process that, you know, requires patience, but it's very much worth it for clarity.
Different Paths: Types of MS
Multiple Sclerosis doesn't, in fact, follow just one single path for everyone. There are various clinical courses, or types, of MS, and understanding these can help people better prepare for what might lie ahead. The most common form, by far, is Relapsing-Remitting MS, often shortened to RRMS. This type is characterized by periods of new or worsening symptoms, called relapses or attacks, followed by periods of partial or complete recovery, known as remissions. During remission, symptoms might lessen or disappear entirely, and the disease activity seems to quiet down, which is, you know, a very welcome break for many.
However, for a significant number of people with RRMS, the disease can, in a way, transition into what's known as Secondary Progressive MS, or SPMS. This happens to about 20% to 40% of people who initially have Relapsing-Remitting MS. With SPMS, there's a steady and gradual progression of symptoms over time, which means that disability slowly but surely increases, regardless of whether there are distinct relapses. This progression can happen, quite simply, with or without periods of remission, and it often occurs anywhere from 10 to 40 years after the initial onset of RRMS, which is, you know, a pretty wide range.
Studies looking into how progressive multiple sclerosis develops have, in fact, largely concentrated on changes within the brain tissue itself, specifically the brain parenchymal changes. This means researchers are trying to understand what's happening at a cellular level that leads to this steady worsening of symptoms, even when there aren't obvious attacks. It's a complex area of research, but understanding these underlying mechanisms is, quite frankly, vital for developing more effective treatments for progressive forms of MS, and that, too, is a big focus for scientists.
There are also other, less common forms of MS, such as Primary Progressive MS (PPMS), where symptoms steadily worsen from the very beginning, without distinct relapses or remissions. Understanding these different types is, you know, important because treatment approaches and expectations can vary significantly depending on the specific course of the disease. Each type presents its own set of challenges, and knowing which path you're on can, in a way, help guide your care and support, and that, too, is something doctors discuss with their patients.
Hope on the Horizon: MS Treatment and Management
For anyone recently diagnosed with Multiple Sclerosis, a very common question, quite naturally, is about new treatment options and whether there's a cure. It's important to know that, as of right now, there isn't a cure for MS. However, this doesn't mean there's no hope. On the contrary, there has been, in fact, significant progress in developing new medications and therapies to manage the condition. The field of drug development for MS has been, quite simply, incredibly active, with new options emerging regularly, and that, too, is a source of optimism for many.
These new treatments, often called disease-modifying therapies (DMTs), aim to slow the progression of the disease, reduce the frequency and severity of relapses, and, you know, sometimes even prevent new lesions from forming in the brain and spinal cord. They work in different ways, often by calming down the overactive immune system that attacks the myelin. Finding the right DMT for an individual can take some time and, quite frankly, a bit of trial and error, as everyone responds differently, and that, too, is something doctors consider carefully.
Beyond DMTs, managing MS also involves a range of treatments to help with specific symptoms. For instance, medications can help with muscle spasms, fatigue, or pain. Physical therapy can be, in a way, incredibly helpful for improving mobility, balance, and strength, which is, you know, especially relevant for those experiencing "ms quad" related challenges like trouble walking. Occupational therapy can assist with adapting daily tasks, making life a little easier, and that, too, is a very practical support.
The goal of treatment is, essentially, to improve a person's quality of life, manage symptoms effectively, and, you know, slow down the disease's impact over time. It's a comprehensive approach that often involves a team of healthcare professionals, including neurologists, physical therapists, occupational therapists, and mental health specialists. This team works together to create a personalized plan that addresses the unique needs of each person living with MS, and that, too, is a very important part of living well with the condition.
Staying informed about new developments in MS research and treatment is, in fact, incredibly empowering. Organizations like the National Multiple Sclerosis Society (Learn more about MS on our site) provide up-to-date information and resources, which are, you know, very helpful for patients and their families. While there's no cure yet, the ongoing progress in drug development offers real hope for better management and, quite simply, a more stable future for many individuals with MS.
Living with MS: Everyday Realities
Living with Multiple Sclerosis means, in fact, learning to adapt to a condition that can, quite literally, change over time. It's a very personal journey, and no two people experience MS in exactly the same way. One of the biggest challenges, you know, can be the unpredictability of symptoms. One day, you might feel relatively good, and the next, fatigue or weakness might make even simple tasks feel incredibly difficult. This fluctuating nature of the condition requires a lot of patience and, quite frankly, a good deal of flexibility.
Adapting to symptoms, especially those affecting mobility like the "ms quad" related issues, often involves practical adjustments. This could mean using assistive devices, like a cane or walker, or making changes around the home to improve accessibility. Physical therapy plays a very important role here, helping people maintain strength, improve balance, and, you know, find new ways to move effectively. It's about finding strategies that work for you to keep living your life as fully as possible, and that, too, is a constant process.
Beyond the physical aspects, the emotional and mental well-being of someone with MS is, quite simply, incredibly important. Dealing with a chronic condition can be emotionally taxing, and it's not uncommon for people to experience feelings of frustration, sadness, or anxiety. Seeking support from family, friends, support groups, or mental health professionals can be, in a way, incredibly beneficial. Sharing experiences with others who understand can provide comfort and, you know, practical advice for navigating daily life.
Managing fatigue, which is a common and often invisible symptom, is, in fact, another key part of living with MS. This isn't just ordinary tiredness; it's a profound exhaustion that can make it hard to concentrate or perform even light activities. Learning to pace yourself, prioritizing rest, and, you know, sometimes adjusting your daily schedule can make a big difference. It's about listening to your body and respecting its limits, which is, quite frankly, a lesson many people with MS learn over time.
Staying informed and actively participating in your own care plan is, quite literally, empowering. Working closely with your healthcare team to monitor symptoms, adjust medications, and explore new therapies helps ensure you're getting the best possible care. Remember, you know, that while MS presents challenges, many people with the condition lead fulfilling and active lives by managing their symptoms and focusing on their well-being. To explore more resources on managing MS, you can Explore our resources on managing MS on our site.
Frequently Asked Questions About MS
Here are some common questions people often have about Multiple Sclerosis:
What are the early signs of MS?
Early signs of MS can, in fact, vary widely, but they often include sensations like numbness or tingling in your limbs, sudden weakness, or trouble with balance and coordination. You might also notice vision changes, such as blurry vision or double vision, or even, you know, a feeling of extreme tiredness that doesn't go away with rest. These initial symptoms can be subtle and, quite frankly, sometimes come and go, making them a bit tricky to identify at first.
How is MS diagnosed?
MS is diagnosed through a combination of methods, since there isn't one single test. Doctors will, quite simply, take a detailed medical history, perform a physical exam to check your reflexes and coordination, and often use MRI scans of the brain and spinal cord to look for characteristic lesions. Sometimes, a spinal tap, which analyzes the fluid around your brain and spinal cord, is also used to gather additional evidence, and that, too, helps confirm the diagnosis.
Can MS be cured?
Currently, there is, in fact, no cure for Multiple Sclerosis. However, there has been significant progress in developing treatments that can help manage the condition. These treatments, known as disease-modifying therapies, aim to reduce the frequency and severity of relapses, slow down the disease's progression, and, you know, manage specific symptoms. While a cure is still being sought, these advancements offer considerable hope for improving the quality of life for people with MS.